
Unknown to most people yesterday, hydroxychloroquine (trade name Plaquenil) is today at the heart of a medical, scientific and ethical issue. Due to the progression of the pandemic, these debates which started in France are now experiencing various developments abroad, notably in the USA where President Donald Trump and Professor Anthony Fauci, director of the National Institute of Allergies and Infectious Diseases , openly oppose.
It all started on February 19, 2020 with a communication from the pharmacology department of the Chinese University of Qingdao mentioning the antiviral activity of chloroquine phosphate in vitro . On March 3, a Chinese team from Guandong Province published a second article reporting the results of treating a small cohort of 30 patients with a daily dose of 400 mg of hydroxychloroquine for 5 days. The primary endpoint was negation of the Covid-19 viral load at the pharyngeal level after 7 days. This study did not mention any significant difference between the treated group and the control group.
While there is currently no consensus data on Covid-19, the history of a potential inhibitory activity of chloroquine (and its derivative, hydroxychloroquine) against coronaviruses is not news. It dates back to the SARS-CoV epidemic in the early 2000s. At the time, several teams described its antiviral activity by in vitro investigations . Back on molecules that have caused a lot of ink to flow.
What is chloroquine?
Chloroquine is produced by chemical synthesis. It is a derivative of quinine, an alkaloid isolated in 1820 by two French pharmacist-chemists, Pierre Joseph Pelletier and Joseph Bienaimé Caventou, from cinchona bark, a shrub native to Ecuador and known under the name of “fever tree” by the Indians of the Andean plateaus.
Chloroquine, originally marketed as Nivaquine, was a central drug in the fight against malaria. It was widely used in the three or four decades following the Second World War, but its interest in this indication has now become anecdotal. In fact, Plasmodium falciparum , the most widespread (and potentially fatal) species of the parasite causing malaria has developed resistance to chloroquine on an almost global scale.
Like any drug, this therapy is not without risk, however: a dose of 2 grams of chloroquine is toxic, while 4 grams constitutes a fatal dose. The development of hydroxychloroquine sulfate, better tolerated by the body, was an alternative, which however remains subject to medical prescription due to its narrow therapeutic margin. This drug is not used as an antimalarial, but it is widely prescribed in certain autoimmune diseases such as lupus disease and rheumatoid arthritis, due to its anti-inflammatory properties. The generally prescribed doses are 600 mg / day for several months.
How do these substances work?
Chloroquine and hydroxychloroquine have numerous and complex therapeutic effects. Their major action is linked to an inhibition of lysosomal functions. Lysosomes are vesicles found in cells and containing enzymes. Active when the pH is acidic, they are able to digest most of the cell’s components: proteins, sugars, lipids, nucleic acids, etc.
What are lysosomes?
Chloroquine was shown early on to have a remarkable affinity for lysosomes. Once concentrated inside, it increases the pH and thus disrupts their enzymatic functions. Scientists have also discovered that chloroquine and hydroxychloroquine stabilize the membranes of endosomes, another kind of vesicle present in the cell and involved in the transit and sorting of molecules.
This property of chloroquine explains its antimalarial effect. In fact, during their life cycle, the parasites responsible for malaria enter red blood cells from which they cut hemoglobin to make their own proteins. They use enzymes contained in a digestive vacuole for this. By accumulating in the latter , chloroquine disrupts the enzymatic functioning, like what happens in lysosomes.
In addition to these effects, chloroquine influences other levels of the body, by inhibiting the functions of effectors of innate (monocytes / macrophages) and specific immunity (lymphocyte activation), or by interfering with certain cellular signaling pathways. These properties are at the origin of its anti-inflammatory effects, which are used to treat autoimmune diseases such as rheumatoid arthritis.
Finally, chloroquine has been shown to interfere with the DNA double helix. It is therefore a relatively toxic compound, presenting a risk of genotoxicity which is mainly expressed during its use in long-term therapy.
The most common side effects during treatment are gastrointestinal manifestations, such as vomiting and diarrhea. Other more serious problems, such as damage to the retina (retinopathy) or the heart (cardiomyopathy) may occur during long-term exposure to chloroquine. In addition, as with many drugs with a narrow therapeutic range, it is also imperative to monitor renal function in the elderly, to avoid overdoses.
Chloroquine interferes with certain microorganisms
Chloroquine and hydroxychloroquine are therefore potentially capable of interfering with the development of microorganisms which infect cells and hijack their lysosomes or endosomes for their benefit.
The efficacy of chloroquine has thus been proven in the treatment of Q fever , caused by the very infectious bacteria Coxiella burnetii , which penetrates into cells and can cause serious heart problems , or Whipple’s disease , due to a another intracellular bacteria , which requires lifelong treatment.
With regard to viruses, things are less clear. In 2005, work carried out on primate cells had demonstrated an in vitro activity on the SARS-CoV-1 virus , responsible for the SARS epidemic of 2003. The SARS-CoV-1 responsible for the disease, having disappeared, the researchers continued to test the activity of chloroquine, in particular on MERS-CoV, with encouraging results in vitro .
On the other hand, other studies had demonstrated a lack of efficacy in vivo on other viruses, such as the chikungunya , dengue , or influenza viruses .
To infect a cell, viruses start by clinging to its surface. In the case of enveloped viruses, that is to say surrounded by a membrane, such as SARS-CoV-2, the next step consists in fusing said membrane with that of the cell . Depending on the virus, this fusion can take place on the cell surface or in endosomes after internalization of the viral particle.
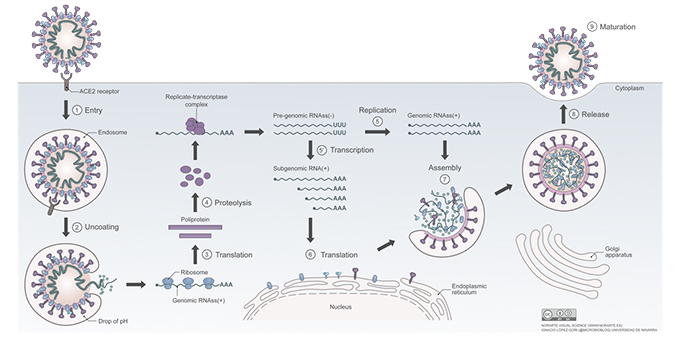
In the case of the SARS-CoV-2 coronavirus, chloroquine could inhibit the fusion of the viral membrane with the cell membrane, thus preventing the passage of the virus into the cytoplasmic compartment . Hydroxychloroquine also inhibits the in vitro replication of SARS-CoV-2 in cell cultures.
Covid-19: is hydroxychloroquine effective?
At this stage of knowledge, it should be noted that it is considered that the transition from the first symptoms of the disease to acute respiratory distress syndrome (ARDS) is most likely due to an uncontrolled release of molecules promoting infection, which would trigger an “inflammatory storm”.
Testing the pharmacological relevance of hydroxychloroquine is therefore not illogical: it could be due to its ability to block the coronavirus and its anti-inflammatory properties. With this in mind, on March 8, 2020, researchers from the Drug Clinical Trial Center in Beijing expressed their interest in the treatment of patients with Covid-19 with hydroxychloroquine rather than chloroquine .
Didier Raoult and his team, at the IHU Méditerranée-infection in Marseille, therefore decided to conduct two preliminary tests. The results of the first of these trials, published on March 20, 2020 , would indicate that an eight-day treatment, combining hydroxychloroquine with a macrolide antibiotic, azithromycin, would lead to “viral clearance” (the virus is no longer detected in patients or in cell cultures). This antibiotic is used because it has been shown that in the case of infection with the influenza A virus (H1N1), it interferes with the process of internalization of the virus . Other studies mention an antiviral action on viruses belonging to the genus Enterovirus .
This work was the subject of various criticisms and discussions as to their methodology : small number of patients, non-randomized trial, absence of control group, etc. In addition, a team from Saint-Louis hospital failed to reproduce results regarding viral clearance .
Other clinical trials on large cohorts will therefore be necessary to find out whether the results observed in vitro translate into interesting effects in vivo and, if this is the case, to assess the risks linked to side effects, to determine the dosage. optimal, indications for this potential drug, etc.
Launched on March 22, the Discovery trial plans to include 3,200 European patients . While hydroxychloroquine was initially excluded, one arm of the trial will now focus on its evaluation, but without combining it with azithromycin. For its part, the Angers University Hospital launched the Hycovid trial , which aims to test the effectiveness of this molecule on 1,300 patients. Finally, the WHO plans to hold a placebo-controlled trial to assess long-term chloroquine prophylaxis . The study would involve 20,000 healthcare workers, with chloroquine being tested daily with the doses used for rheumatoid arthritis.
Except huge surprise, it will probably be necessary to wait several more weeks before knowing with certainty if the results of the first Chinese and French communications, which related to small numbers of patients, will be confirmed (or not) on larger series.
Author Bio: Emmanuel Drouet is a Pharmacist, Doctor in Human Virology, University of Grenoble Alpes
